Comments
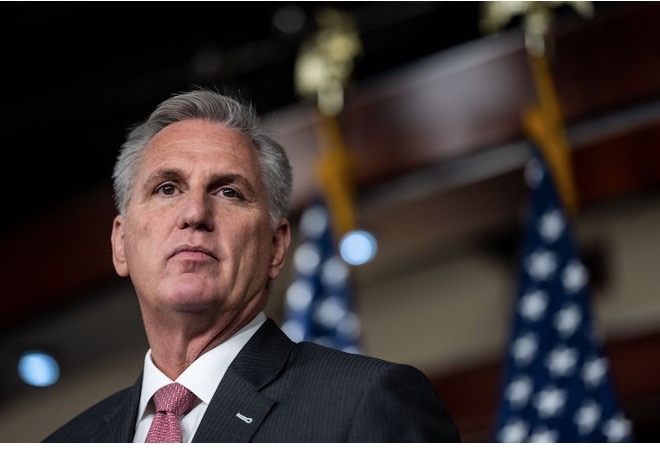
DEBT CEILING - A Republican proposal led by House Speaker Kevin McCarthy would take Medicaid coverage away from people who do not meet new work-reporting requirements. The McCarthy proposal would apply to all states, but in practice it would heavily impact people covered by the Affordable Care Act (ACA) Medicaid expansion. Of this group, more than 10 million people in Medicaid expansion states would be at significant risk of losing coverage under the McCarthy proposal. This group would be subject to the new Medicaid requirement, and they are not part of a group that states could readily identify in existing data sources and exclude from burdensome reporting. The McCarthy proposal could jeopardize coverage for millions more, by prompting some states to drop the ACA Medicaid expansion or dissuading states that have not yet taken the expansion from adopting it.
Nationwide, we estimate that over 10 million Medicaid expansion enrollees — more than 1 in 5 of all Medicaid enrollees in expansion states — would be at risk of losing Medicaid coverage under the policy in McCarthy’s debt limit bill, using 2019 (pre-pandemic) data. Some 74 percent of all expansion enrollees and 21 percent of all Medicaid beneficiaries in the states that have adopted the expansion would be subject to the new requirements and, thus, at risk of losing coverage.
People in every expansion state would be affected, with the share of total Medicaid enrollees at risk ranging from 15 to 37 percent. (See Table 1 and Methodology.) Because we use 2019 data, the national estimate does not include the nine states that expanded coverage after that date and therefore very likely understates the number of enrollees at risk. If those states were included, it would likely add upward of 1 million more enrollees at risk of losing coverage.
While not all of those at risk under McCarthy’s proposal would lose coverage, many would, including people who are working or are eligible for an exemption but would be disenrolled due to administrative burdens and red tape.[2] This was the experience in Arkansas, which is the only state that briefly took people’s Medicaid coverage away for not meeting work-reporting requirements, until a federal court halted the program following massive coverage losses. In just seven months of implementation, some 18,000 people — 1 in 4 subject to the requirements — lost coverage. Moreover, research found that the new requirements had no impact on employment outcomes. The McCarthy Medicaid provision draws heavily from the failed Arkansas experiment but is harsher in some respects, applying to somewhat older adults, for example.
The more than 10 million estimate (looking just at the states that had expanded Medicaid prior to 2019) does not fully account for the sweeping impact the Medicaid work-reporting requirement could have. For example, while the bill directs states “whenever possible” to use electronic data sources to verify whether people meet the criteria for continued Medicaid coverage, the extent to which this would protect people from losing coverage or from onerous reporting would depend on implementation decisions at both the federal and state level.
Proponents of the new requirements argue that they give states an option to take Medicaid coverage away from people who don’t comply with the new work-reporting requirement. This is misdirection at best.
The bill terminates federally funded Medicaid coverage for those who don’t meet the work-reporting requirements. In theory, states could provide fully state-funded coverage to those whose federal Medicaid coverage is taken away, but with the federal government currently covering 90 percent of the cost of coverage for expansion enrollees, states are exceedingly unlikely to continue coverage for large numbers of people who don’t meet the requirement. (It is worth noting that states did not provide state-funded coverage for this group prior to the ACA’s expansion, though they were able to do so.)
Moreover, administering these new requirements would be complicated for state and local governments, which would have to pick up a significant portion of the costs associated with implementing the complex systems to verify work, determine who meets automatic exemption criteria (such as those with children), and assess applications for exemptions based on criteria, such as an illness, that the state doesn’t know through its eligibility system.
States also would have to absorb the costs associated with higher caseload churn — that is, people losing coverage and then having to reapply or seek to have their coverage reinstated, all processes that require caseworker staff time. And uncompensated care costs would increase because people have lost coverage, adding further to the costs that states and safety net health care providers would have to pick up.
Without a doubt, adding work-reporting requirements to Medicaid would cause many low-income adults to lose coverage due to bureaucratic hurdles and would leave people without the health care they need, including life-saving medications, treatment to manage chronic conditions, and care for acute illnesses. People’s access to health care and other basic supports, such as housing, food, or child care, should not hinge on whether they meet a work-reporting requirement or successfully navigate a complicated system to either report work hours or claim an exemption.[3]
McCarthy Medicaid Provision Builds on Failed Arkansas Experiment
The Arkansas plan, implemented in 2018, required that Medicaid expansion enrollees aged 19-49 document at least 80 hours of work or other qualifying activities (e.g. job training, volunteering) per month.[4] Exemptions were available for various groups including pregnant people, certain types of caregivers, and people with certain health conditions, but qualifying for these exemptions required that enrollees successfully navigate the reporting system or that the state use available data to determine exemption status. As a result, more than 18,000 people (about one-quarter of those subject to the requirements) lost coverage in just seven months, before a federal court blocked the policy.[5]
The McCarthy plan is similar to Arkansas’ but applies to a broader set of Medicaid enrollees. First, it applies to enrollees aged 19-55, a wider age range that includes more older adults. Second, it is not explicitly limited to Medicaid expansion enrollees, unlike the Arkansas policy. While all states would have to set up new processes to validate exemptions, we assume that because existing state data sources could readily be used to exempt the bulk of Medicaid enrollees who are not part of the expansion group, the impact would be largely on expansion enrollees.[6] Third, some groups exempt under the Arkansas plan, including postpartum people, people identified as “medically frail,” and people receiving unemployment benefits, are not exempt under the McCarthy plan.
A KFF study estimated that under a nationwide Medicaid work-reporting requirements policy similar to policies implemented in Arkansas and proposed by other states, most people losing coverage would be complying with or exempt from the requirements but would be disenrolled due to administrative burdens and red tape.[7] Using conservative assumptions about disenrollment based on a survey of the research literature, the study found that 62 to 91 percent of those losing coverage would be people who qualify as eligible under the policy. Coverage losses would be concentrated among those eligible because the overwhelming majority of Medicaid enrollees already meet the requirements or an exemption criterion, yet they would still be at risk due to the bureaucratic complexity of reporting and proving exemption status.
Overall, between 1.4 and 4 million people would have lost Medicaid coverage if Medicaid work-requirements were imposed in 2016, the KFF study estimated.[8]This estimate is roughly in line with the Congressional Budget Office’s projection that a nationwide policy similar to Arkansas’ would result in a reduction in Medicaid enrollment of 2.2 million adults per year for the 2023-2031 period.[9]
Our analysis is not a projection of the number of people who will lose coverage, but rather shows that more than 10 million people would be subject to these requirements and, thus, at risk of losing coveragefrom a policy that would erect burdensome requirements to report work or claim exemptions. A large share of the 10 million people subject to the requirements would have to navigate complex work-reporting and verification systems each month while others would have to navigate the exemption process periodically to retain coverage.
Research suggests that some populations would be especially harmed by these work-reporting requirements, including people with disabilities, women, people who are experiencing homelessness, and people with mental health conditions or substance use disorders.[10] Even though exemptions would apply to some in these groups, states often lack the capacity to hire sufficient staff to respond to people’s questions or manage work-reporting systems and the exemption process. People who have fewer transportation options or live in rural areas,[11]face language or literacy barriers, are in poor health or have limited mobility, or have limited internet access[12] would face particular barriers to understanding the new requirements and navigating reporting systems, applying for exemptions, and collecting the verification needed to prove that they meet an exemption criterion.
There is no upside to Medicaid work-reporting requirements. Research has not found any impact of the requirements on employment,[13] and data from Arkansas show that few enrollees engaged in new work-related activities.[14]Instead, work-reporting requirements strip health coverage from people with low incomes — most of whom are already meeting or exempt from the requirements — leading to gaps in care that damage their health and financial security and make it harder for them to find or keep a job.[15]
In this paper and in Table 1 below, we estimate the number of Medicaid expansion group enrollees at risk of losing coverage using administrative data on Medicaid expansion enrollment for 2019, combined with American Community Survey (ACS) data and state enrollment policies.
We use 2019 Medicaid expansion group enrollment to avoid including the large increase in Medicaid enrollment that began in 2020 as a result of the requirement that Medicaid provide continuous coverage during the public health emergency. This continuous coverage requirement ended on March 31, 2023, and while estimates of coverage loss during the unwinding of the requirement are highly uncertain, enrollment declines are potentially large.[16]By using 2019 data, we avoid overstating our estimates of expansion enrollees at risk in each state once unwinding is complete.
|
TABLE 1 |
|||
|
Estimated Number of Medicaid Expansion Enrollees Whose Coverage Would Be at Risk Under McCarthy Medicaid Work-Reporting Requirements Proposal |
|||
|
Number of Medicaid expansion enrollees at risk of losing coverage |
Share of all Medicaid enrollees |
||
|
Alaska |
40,000 |
19% |
|
|
Arizona |
316,000 |
17% |
|
|
Arkansas |
156,000 |
19% |
|
|
California |
2,673,000 |
22% |
|
|
Colorado |
290,000 |
24% |
|
|
Connecticut |
226,000 |
24% |
|
|
Delaware |
46,000 |
22% |
|
|
District of Columbia |
96,000 |
37% |
|
|
Hawai’i |
81,000 |
26% |
|
|
Illinois |
562,000 |
21% |
|
|
Idaho |
Data not available |
Data not available |
|
|
Indiana |
204,000 |
15% |
|
|
Iowa |
132,000 |
22% |
|
|
Kentucky |
269,000 |
21% |
|
|
Louisiana |
287,000 |
18% |
|
|
Maine |
Data not available |
Data not available |
|
|
Maryland |
235,000 |
19% |
|
|
Massachusetts |
288,000 |
17% |
|
|
Michigan |
464,000 |
19% |
|
|
Minnesota |
153,000 |
15% |
|
|
Missouri |
Data not available |
Data not available |
|
|
Montana |
60,000 |
24% |
|
|
Nebraska |
Data not available |
Data not available |
|
|
Nevada |
137,000 |
24% |
|
|
New Hampshire |
36,000 |
20% |
|
|
New Jersey |
411,000 |
26% |
|
|
New Mexico |
174,000 |
21% |
|
|
New York |
1,287,000 |
21% |
|
|
North Dakota |
15,000 |
17% |
|
|
Ohio |
421,000 |
15% |
|
|
Oklahoma |
Data not available |
Data not available |
|
|
Oregon |
316,000 |
33% |
|
|
Pennsylvania |
519,000 |
18% |
|
|
Rhode Island |
55,000 |
19% |
|
|
Utah |
Data not available |
Data not available |
|
|
Vermont |
47,000 |
29% |
|
|
Virginia |
Data not available |
Data not available |
|
|
Washington |
371,000 |
21% |
|
|
West Virginia |
101,000 |
19% |
|
|
Total |
10,470,000 |
21% |
|
|
Adopted expansion but not yet implemented: |
|||
|
North Carolina |
Data not available |
Data not available |
|
|
South Dakota |
Data not available |
Data not available |
|
Methodology
As stated above, our estimates are based on a combination of administrative data on Medicaid expansion enrollment, ACS data, and state enrollment policies.
Because our data are based on 2019 (pre-pandemic) Medicaid expansion enrollment, they do not include expansion enrollees at risk in states that expanded in 2019 or later, including Idaho, Maine, Missouri, Nebraska, Oklahoma, Utah, and Virginia. We also cannot produce expansion group estimates for North Carolina and South Dakota, which have enacted but not yet implemented expansion. Our national total estimate is therefore likely to understate the number of enrollees at risk. Finally, by shifting costs to states, the McCarthy proposal could result in some states deciding to drop the ACA Medicaid expansion, jeopardizing coverage for millions more. Similarly, these new requirements could dissuade some states that have not yet adopted the expansion from doing so.
We consider Medicaid expansion enrollees aged 19-55 and exclude from this group people who live with dependent children aged 0-17. States should be able to exclude this group automatically (without requiring them to apply for an exemption) using existing administrative data, so they are less likely to be at risk.
We do not estimate other exemptions or work status because these individuals would be more likely than parents to have to report their employment or earnings monthly or to apply for and submit documentation to receive an exemption. Research indicates that most people who would lose coverage under work-reporting requirements would be disenrolled despite working or qualifying for an exemption due to the complexities of proving that they are working or meet an exemption criterion.
Publicly available administrative data on Medicaid expansion enrollees do not include detailed enrollee characteristics. We therefore use data from the U.S. Census Bureau’s American Community Survey as well as state-level eligibility rules to estimate the share of expansion enrollees who are aged 19-55 and who do not have dependent children in each state.
(Gideon Lukens is Senior Fellow and Director of Research and Data Analysis on the Center on Budget and Policy Priorities' Health Policy team, where he works on Medicaid, health insurance exchanges, and other policy issues. This article was on CommonDreams.org.)