Comments
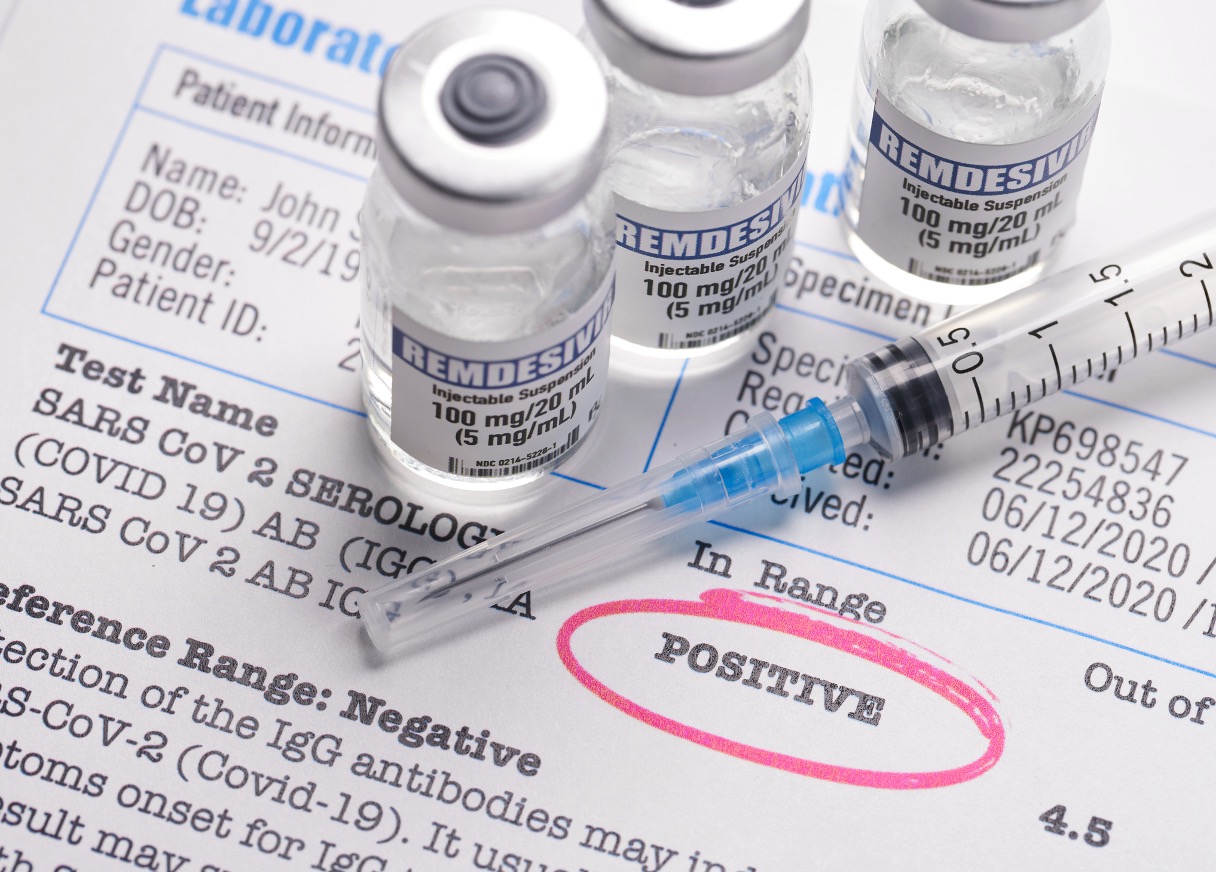
GELFAND’S WORLD - I recently found myself with a nagging, hacking cough -- where one cough leads to another leads to another ad nauseum -- and much to my surprise, found that I was having a second case of Covid. In this new, modern day, I was offered an effective antiviral drug which could be called in at my pharmacy, or I could just maintain with Tylenol and cough syrup. There was no concern on the part of the providers that I would end up on a ventilator and drop dead.
And it occurred to me that Anthony Fauci, Gavin Newsom, and the CDC had been exactly right.
Considering the arguments you might hear from Republican presidential candidates and their supporters, this is a legitimate topic to bring up. The Governor of Florida, for one, would like to pretend that relaxing all of the anti-Covid precautions was the right thing to do. His appointed state Surgeon General has gone even further by pushing the antivaccine line.
Let's go back to the early days of the pandemic and consider three critical issues which came up at the time:
1) Is this thing capable of killing people?
2) What do we know about how it is spread?
3) How robust is our knowledge about the spread and about treatments?
It turns out that the third element was critically important at the time. Let's consider a prime example. One doctor suggested, based on relatively limited evidence, that using one drug -- which would not have been thought of as being an effective antiviral -- had a modestly better survival rate than conventional therapy. There was a published paper to this effect. Much later, scientists who carefully looked at the paper concluded that some of the data was likely made up.
You got that -- fabricated, as in invented out of whole cloth, and not coming from measurements of patient survival in the hospital.
So, this was an example of an unlikely result supported by inadequate evidence, and which could not withstand further investigation.
You had a drug which doesn't really have much effect on viral infections, but was tried out by one researcher who applied his own wishful thinking to the results and then skewed the results.
On the other hand, the modern antiviral drug has been tested repeatedly.
One last point on the idea of robust results: You can get a better idea of how robust an effect is by the use of statistics in competently designed and skillfully carried out experiments. The people who do these sorts of experiments and engage in data analysis have to be willing to admit when the results don't support their pet theories. The medical literature is full of such disappointing results.
Question 1 -- is the virus deadly -- became obvious, and rapidly so. The virus was killing people by the thousands.
Question 2 -- how it is spread -- was less obvious at the beginning. Do we get it from sneezing on each other, or by shaking hands, or by turning a doorknob that had previously been contaminated? Were healthcare workers susceptible to catching the disease after treating a patient?
This can be a challenging question for those who do research on infectious diseases. Those of a certain age may remember that when AIDS was first recognized as a disease, there was a lot of conjecture as to what its cause might be. One well known professor in the Bay Area suspected that AIDS patients were immunocompromised due to their use of chemical stimulants. Others suspected a viral origin, but had limited knowledge as to the actual mode of transmission.
Things were somewhat different for Covid-19. In early 2020, science had robust knowledge that there was a new and deadly disease and that it was caused by a particular virus. But whether the virus could be spread to humans by a cough or a sneeze, or by fecal contamination, or by some other route such as virus landing on a counter top was essentially unknown at the moment. It didn't hurt to recommend hand washing and the use of disinfectants, although it had not been shown whether these would help. Notice that as information developed, recommendations on things like the use of hand wipes lessened.
In short, the fact that a deadly disease was produced by a newly discovered virus was known in detail. There were, to be sure, fine points such as the propensity of the virus to mutate during human infections, but there really wasn't any question about the nature of the infectious agent.
Exponential Growth
The term "exponential growth" is one of the more misused terms. Properly used, it implies that the number of cases doubles over a certain amount of time, and then -- in approximately the same amount of time -- it double again. Then it doubles once more, and so on.
Interestingly (and in a very scary way) you could track the number of Covid-19 cases from month to month. During the middle of 2020, you could track the various reports of case numbers and see that they were doubling approximately every two weeks.
Think of it like this: 200, 400, 800, 1600, 3200 . . .
In the real world, the numbers were a bit rougher, but it was amazing how close to pure exponential growth we were seeing at the time.
Predicting the outcome of an exponentially growing disease over the course of time
Nothing can grow exponentially forever. The disease will run out of people to infect. At the point that the disease has already infected half the population, the number of new cases is going to slow down. But a lot of people will have been sick or will have died by the time we get to that point.
Interrupting the exponential growth
Think of the position government scientists and planners faced during the early days of 2020. For every 1000 cases of Covid-19, a certain number of people would -- on average -- die. On the other hand, if somebody could come up with a vaccine, we could put a stop to the dying.
Was there some way to cut down on the exponential growth of the epidemic at least for a while, in the hope that a vaccine would be perfected? That's the idea of "flattening the curve."
Think of the case load as being in the shape of a bell curve, where there were very few cases in April of 2020, but by October there were a lot more. Imagine the curve as hitting a peak in the middle of 2022. By that time it would have resulted in a couple of million dead.
Now imagine if the curve could be stretched out -- way out -- so that it only doubled every month or two. By the middle of 2021, there would still be a lot of dead people, but a lot less than if we did nothing. That's what was meant by "flattening" the curve -- causing it to grow more slowly, and to a lesser extent. The bell curve would be a lot wider, but would be lower. If we never got a vaccine, then it still might kill as many people overall, but it would take longer. But if we could develop a vaccine, then lots of lives would be saved, simply because we had not gone so far along the bell curve of infection and death.
So that's where we were in the early part of 2020: A deadly disease, growing exponentially, and not a lot known about how it got from one person to the next. Maybe it could be spread by touching a table top -- would this virus live very long exposed like that? And we didn't have much in the way of remedies.
The one thing that was likely to be true was that keeping people separated from each other would likely help. The virus was being spread somehow, and reducing all possible means of spreading was the best available approach at the time.
Was this approach going overboard for some possible routes of spreading? Undoubtedly. But think of the logic -- If we are parsimonious in cutting down on human transmission, then we will be letting a larger number of infections get through. Are children more resistant? Possibly, but we weren't actually sure at the beginning how much more resistant.
So governmental leaders were left with a politically difficult decision. Closing shopping malls and public schools would undoubtedly lead to public resentment. Telling people that they should mask should have been a lot easier, but was used as a symbol of oppression by the other side. My view is that the governor of California and the mayor of Los Angeles did good jobs in keeping the people informed and in enforcing rules that were generally reasonable.
They were guided by Anthony Fauci and his colleagues at the CDC.
In a moment where complete information was not available, they all did a good job in reducing the immediate death toll and vastly reducing the ultimate death toll. They had to juggle their responses to fit the best available data, but that's where the robustness issue was paramount. You had to be really sure about relaxing some rule before doing so.
They knew that keeping people separated would reduce disease transmission -- this is a robust finding. There was no robust data supporting keeping public schools open, just as there was little data about the Covid death toll if schools were kept closed.
In this situation, the government officials who were being responsible did their best to minimize the casualties while allowing for relaxed standards as new data became available. But the new data also had to be competently generated.
It's been four years since the epidemic began, quickly escalated to pandemic proportion, and has gradually eased. It is still killing people in Los Angeles County, but at a rate of 2 - 5 people per day, rather than the much higher numbers of two and three years ago.
In this election year of 2024, we can consider that the politicization of the Covid-19 vaccine was a terribly unfortunate factor in this post-vaccine world. Political scientists and epidemiologists have found that Trump-voting counties had considerably higher numbers of Covid deaths per capita compared to Biden-voting counties. Here in California and at the CDC, good decisions were made and proper advice was given. The fact that I can survive a second bout of the Covid, quite possibly due to the resistance given me by the vaccine, is something to consider.
(Bob Gelfand writes on science, culture, and politics for CityWatch. He can be reached at [email protected].)